Joint pain often manifests itself in very different ways in everyday life. There can be various causes behind individual complaints. You can read about the possible causes below.
In principle, all visits to our private practice for orthopaedics & traumatology in Frankfurt are based on a detailed discussion about the cause, course, treatment options, etc. as well as a thorough physical examination. Only when the patient correctly understands their clinical picture can they support the treatment path with conviction.

Dr. med. Nader Tabrizi

Dr. med. Stefan Chwalek

Dr. med. Isabella Gruber
This is a chronic, degenerative disease of the joints in which the cartilage covering the joint surfaces is gradually broken down by the body.
Articular cartilage plays an important role as a smooth, cushioning layer that separates the bones from each other and thus ensures smooth movement of the joints. If this cartilage is damaged during the course of osteoarthritis, the bones rub directly against each other. This can cause pain and functional disorders.
Osteoarthritis is a so-called “wear and tear disease”, which means that it often occurs in connection with the ageing process. However, it is not exclusively caused by age.
Several factors can contribute to its development, including mechanical stress, years of overuse of joints and genetic predispositions.
There are various circumstances that can promote the development and progression of joint wear and tear. These influence both the risk of developing osteoarthritis and the severity of the disease. The most important risk factors are
- Age
The risk of osteoarthritis increases considerably with age. The joint cartilage wears out over the years due to constant stress. The cartilage’s ability to regenerate also decreases with age, which can lead to progressive damage. - Overweight
A higher body weight means more strain on the joints. This causes the cartilage to wear out more quickly. In addition, fatty tissue can produce pro-inflammatory substances that further accelerate the breakdown of cartilage. As a rule, knee and hip joints in particular suffer from the effects of excess weight. - Joint injuries
Previous injuries, such as cruciate ligament ruptures, meniscus damage or bone fractures in the joint area, increase the risk of osteoarthritis. Even if the injuries have healed completely, the cartilage may be more susceptible to wear and tear due to the previous damage. - Overloading the joints
Chronic overloading due to monotonous or one-sided physical movements can put a lot of strain on the joints. This mainly affects people who work in occupations involving heavy physical strain (e.g. construction workers or athletes). - Genetic predisposition
Genetic factors also play an important role in the development of osteoarthritis. People whose close relatives are affected by joint wear and tear have an increased risk of developing the disease themselves. - Misalignment of the joints
Congenital or acquired misalignments of the joints, such as bowlegs or knock-knees, put uneven strain on the body. As a result, certain parts of the joint cartilage can wear out more quickly. - Muscle weakness
If the muscles are insufficiently trained, they cannot adequately stabilize and protect the joints. Weak thigh muscles play a role in knee osteoarthritis, for example, as they are unable to relieve the joint sufficiently. - Inflammations
Chronic inflammation in the body, also caused by autoimmune diseases such as rheumatoid arthritis, can promote joint and cartilage damage. Although osteoarthritis itself is not primarily an inflammatory disease, inflammatory processes can promote cartilage degradation. - Metabolic diseases
Certain metabolic diseases such as diabetes mellitus and gout also increase the risk of joint wear and tear. Insulin resistance and elevated uric acid levels can trigger inflammatory processes.
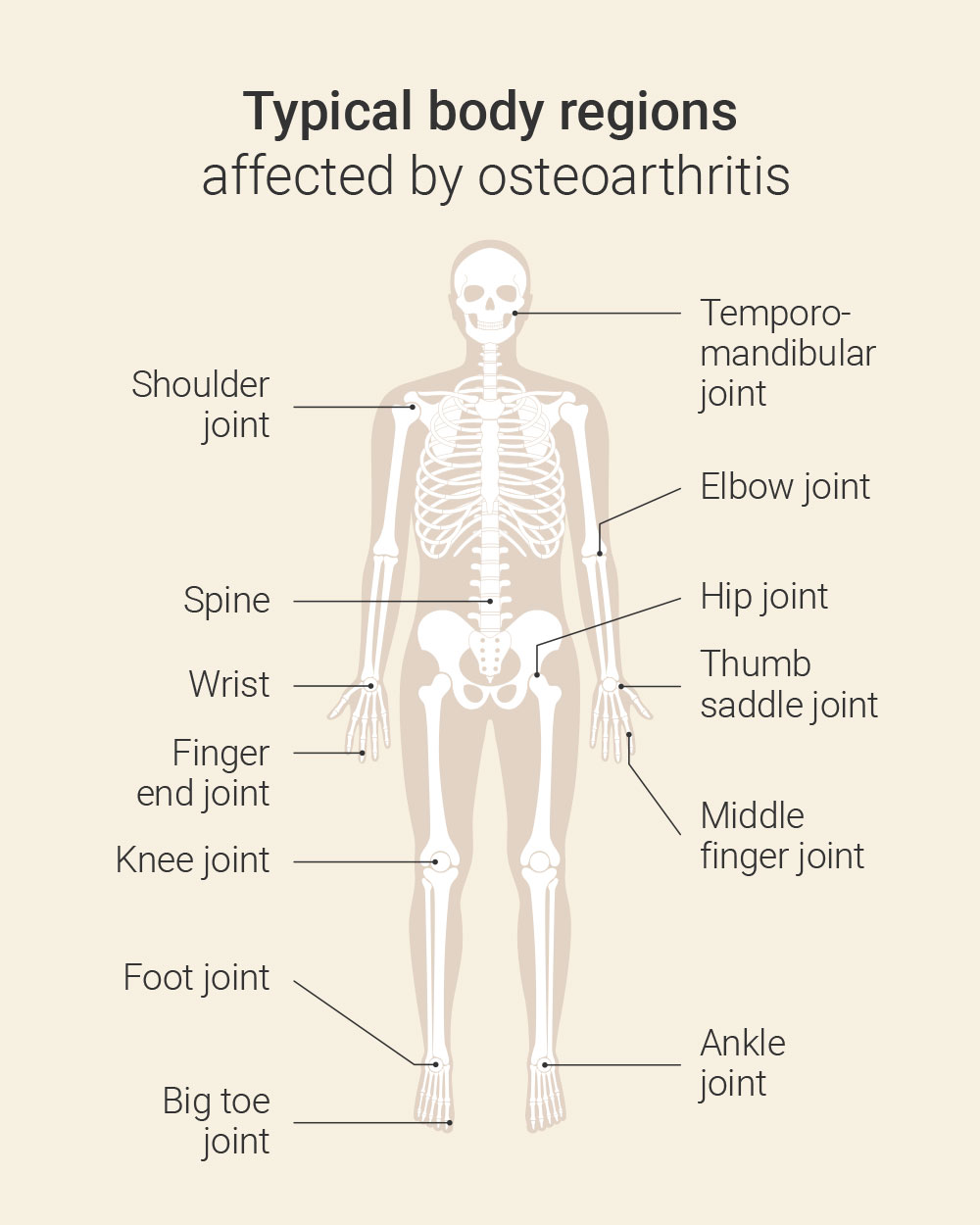
- Knee joint (gonarthrosis)
- Hip joint (coxarthrosis)
- Shoulder joint (osteoarthritis of the shoulder)
- Spine (spondylarthrosis)
- Finger end joints (Heberden’s osteoarthritis)
- Middle finger joints (Bouchard arthrosis)
- Thumb saddle joint (rhizarthrosis)
- Ankle joint (ankle arthrosis)
- Big toe joint (hallux rigidus)
- Elbow joint (elbow arthrosis)
- Temporomandibular joint (temporomandibular joint arthrosis)
- Wrist (wrist arthrosis)
- Foot joints (talo-crural arthrosis)
The symptoms that joint wear and tear can cause often develop gradually and worsen over time – the more advanced the wear and tear of the cartilage, the more severe the associated symptoms often are. The following signs and symptoms are typical of the condition:
- Pain
Painful discomfort in the affected joints is the most common symptom of osteoarthritis. It initially occurs during exertion, for example when walking, climbing stairs or lifting weights. It usually subsides at rest. At an advanced stage, the pain can also occur at rest or at night. - Stiffness
Joint stiffness often occurs after periods of rest or in the morning after waking up (morning stiffness). This stiffness usually lasts less than 30 minutes and improves with movement. As the disease progresses, however, the joint stiffness can last longer and become more severe. - Restriction of movement
In the advanced stages of osteoarthritis, the mobility of the affected joint becomes increasingly restricted. This affects the ability to fully bend or extend the joint as well as general movements such as walking, reaching or standing up. - Grinding and rubbing in the joint (crepitation)
When moving the affected joint, a grinding, clicking or rubbing noise may occur. This noise occurs when the cartilage-covered joint surfaces are no longer smooth and bone meets bone. - Swelling
Sometimes the affected joint can swell. This swelling can be caused by an accumulation of fluid in the joint (joint effusion) or by irritation of the surrounding soft tissue. In advanced osteoarthritis, bone outgrowths (osteophytes) can also lead to swelling. - Heat and redness
In some cases, especially when inflammation occurs in the joint, the affected joint may be warm and reddened. However, these inflammatory episodes are less common in osteoarthritis than in other joint diseases such as rheumatoid arthritis. - Changes in the shape of the joint
Advanced osteoarthritis can lead to visible changes in the shape of the affected joint. These are caused by bone outgrowths (osteophytes) that form at the edges of the joint, as well as by the reduction of cartilage and the displacement of joint structures. - Muscle wasting
By protecting the painful joint, the muscles of the surrounding musculature often break down as they are used less (atrophy). This can further increase the load on the joint and worsen the symptoms. - Fatigue
People with osteoarthritis often feel exhausted more quickly, as the constant pain and restricted movement are exhausting and stressful. This lack of energy can have a significant impact on quality of life. - Altered gait pattern
Osteoarthritis in the lower extremities can lead to an altered gait pattern. This is because those affected try to relieve the painful joint. This results in a relieving posture. - Weather-related complaints
Many patients that we treat in our private practice for orthopaedics & traumatology in Frankfurt report a worsening of symptoms in damp or cold weather. The exact reasons for this are not fully understood, but could be related to changes in air pressure and the temperature sensitivity of the joint.
The intensity and progression of these symptoms can vary greatly from person to person. Some sufferers experience only mild symptoms for years. In others, joint wear progresses rapidly and causes more severe symptoms.
There are various forms of osteoarthritis, which can be categorised according to different criteria. Classification is usually based on the affected joint, the cause of the disease and the degree of severity. Here are the most important forms:
- Primary osteoarthritis
It develops without any recognisable external cause. It is often associated with the ageing process, in which the cartilage gradually wears away. Genetic factors, hormonal influences and age-related changes to the joints also play a role. Primary osteoarthritis usually affects several joints at the same time and often occurs in the knees, hips, hands and spine, as these body structures are generally subjected to more stress. - Secondary osteoarthritis
Secondary osteoarthritis develops as a result of other diseases or injuries. Specific causes that accelerate the degradation of the cartilage can be recognised here, such as- Joint injuries (e.g. fractures, torn ligaments, meniscus damage)
- Malpositions (e.g. knock knees or bow legs)
- Metabolic diseases (e.g. gout or diabetes)
- Overweight or occupational overloading of the joints
- Inflammatory joint diseases (e.g. rheumatoid arthritis)
- Localised osteoarthritis
Here, only a single joint or a small group of joints is affected. Examples of localised osteoarthritis are- Gonarthrosis
- Coxarthrosis
- Omarthrosis
- Generalised osteoarthritis
Several joints are affected at the same time. This often occurs as part of primary osteoarthritis. Generalised osteoarthritis is often associated with a genetic or hormonal background. - Inflammatory osteoarthritis
In some cases, cartilage degradation can develop inflammatory episodes, which can be accompanied by pain, swelling and a significant worsening of symptoms. These flare-ups are not as common as with other inflammatory joint diseases, but can occur during the course of osteoarthritis. - Erosive osteoarthritis
This rarer, more aggressive form of the disease mainly affects the fingers. It is characterised by the breakdown of cartilage and damage to the underlying bone and can lead to significant deformities of the fingers.
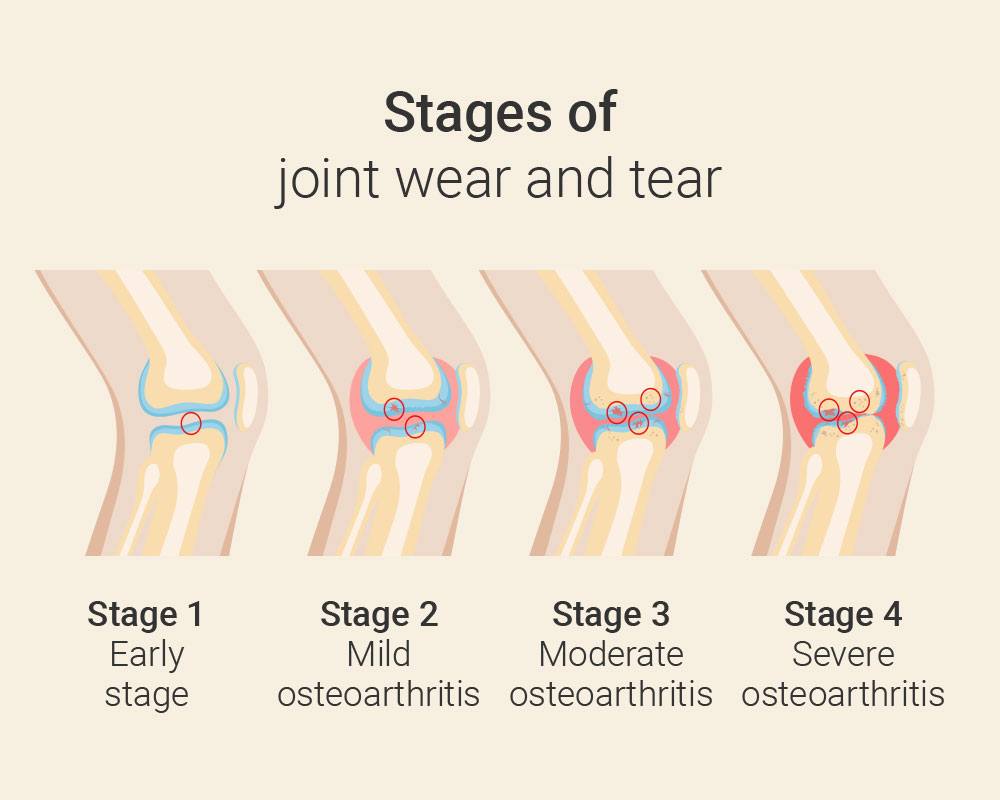
Osteoarthritis can be categorised into different stages according to its severity. This categorisation is generally based on the degree of cartilage damage and the associated changes in the joint.
- Stage 0: No osteoarthritis
The joint shows no signs of change. The joint cartilage is intact. There is no pain or restrictions. - Stage 1: Early stage
Slight changes occur in the joint (e.g. minimal bony growths). The affected cartilage also shows the first slight signs of wear. However, the joint space is still largely normal. Symptoms are hardly or only slightly pronounced. Those affected occasionally notice slight joint stiffness or discomfort with heavy loads. - Stage 2: Mild osteoarthritis
Now there are noticeable but moderate bony changes and a slight narrowing of the joint space. The cartilage begins to break down, but there is still a certain protective layer. At this stage, there is often mild to moderate pain and occasional stiffness – especially after periods of rest or heavy exertion. Initial movement restrictions may also occur. - Stage 3: Moderate osteoarthritis
The cartilage damage is now clear. There is pronounced osteophyte formation and a significant narrowing of the joint space. The affected cartilage is clearly worn away. The bone under the cartilage is increasingly stressed. Pain is now frequent, even at rest. Stiffness and limited mobility increase. Swelling or rubbing in the joint may also occur. - Stage 4: Severe osteoarthritis
There is now a severe degenerative change in the joint with very pronounced osteophytes. The joint space has narrowed considerably or even completely. The cartilage is almost completely degraded and the bone underneath is severely affected. The bones rub directly against each other and bone changes such as sclerosis or cyst formation occur. Those affected suffer greatly, often permanently, from pain, even at rest. Movement is severely restricted. Furthermore, there are often joint deformities and significant swelling. Patients often find it difficult to perform everyday tasks.
A “clean” diagnosis is important for successful therapy. In order to maintain this, a detailed medical examination, a thorough physical examination and purposeful diagnostics are required. From this, a concept for treatment is defined together.
Anti-inflammatory substances are used for painful overload or mis-loading syndromes as well as wear phenomena. These are usually injected into the affected joint or into the surrounding soft tissues (for example, joint capsules, band structures, bursa sacs, etc.).
Infiltrations are targeted injections that can relieve pain and inhibit inflammation. There are two main types:
- Periarticular infiltrations
These are injected into the tissue around the joint, e.g. in muscles, tendons, ligaments or bursae. This can reduce local inflammation and tension. - Intra-articular infiltrations
Here we administer the injection directly into the joint space to improve gliding and protect the cartilage. Typical active ingredients are cortisone (anti-inflammatory), hyaluronic acid (lubricating effect) or PRP (platelet-rich plasma for regeneration).
These treatments can effectively alleviate osteoarthritis pain and improve the mobility of the affected joint.
In the so-called self-blood therapy, certain corporeal blood cells (especially blood platelets) are injected into inflamed tissues or joints. The healing effect of rich plasma is due to the growth factors that are released from them and induce a wound healing reaction. Numerous studies have shown success in osteoarthritis or tendon inflammations.
Autologous blood therapy for osteoarthritis, also known as PRP therapy (platelet-rich plasma), is a regenerative procedure that can promote healing and cartilage protection in the joint. The therapy is particularly suitable for patients with early to moderate stages of osteoarthritis and offers a natural alternative to cortisone or hyaluronic acid.
For PRP therapy, we take a small amount of your blood, process it in a special centrifuge and inject the concentrated plasma directly into the affected joint.
The plasma contains growth factors. These are the body’s own proteins that play a central role in cell regeneration and tissue healing. Growth factors activate cells that renew cartilage and other tissue structures. They also support the formation of new blood vessels, which improve the supply of nutrients to the tissue. The special proteins also slow down the breakdown of cartilage cells and can therefore slow down wear and tear. They also have the ability to reduce inflammatory processes in the joint and thus alleviate pain.
As we obtain these growth factors from your own blood, they are particularly well tolerated and offer a natural way to support the healing and function of the joints.
In arthrotically modified joints, movement is very important in order to produce sufficient joint lubrication but also to stimulate the metabolism within the joint. The stronger the joint-stabilizing musculature is, the less the joint cartilage surface is subjected to pressure loads. The maintenance of optimal joint function with respect to the soft tissues (joint capsule, tendons, ligaments, etc.) is vital.
For a variety of injuries, inflammations or instabilities, for example, orthopedic devices can provide temporary or permanent relief. Depending on the situation and necessity, such medical devices can be prescribed, and their use and duration of use are determined together.
The principle is based on a relaxing or stabilizing effect on the muscles or joints, depending on the technique and the material used. The effect in the muscles or joints is mediated via the skin and the subcutaneous tissue. Kinesio-Taping has been widely used in recent years, but has been used in orthopedics since the 1970s. It was developed by the Japanese chiropractor Kenzo Kaser.
More information at: Kinesio Taping Frankfurt
Body-specific pain-inhibiting systems are activated by needles in defined skin regions. The origin of this practice dates back to 200 years before Christ.
Osteoarthritis of the knee: When the cartilage in the knee joint wears out
Dealing with the signs and causes of these joint changes at an early stage is crucial in order to alleviate symptoms and maintain mobility for as long as possible.
Secondary osteoarthritis: what you need to know
It becomes particularly challenging when osteoarthritis is not caused by natural ageing processes, but as a result of another disease or injury. But how can you recognize this so-called secondary osteoarthritis?
Difference osteoarthritis and arthritis
Osteoarthritis is one of the most common joint diseases, causing the destruction of the cartilage layer of a joint. Arthritis, on the other hand, is an inflammatory joint disease that can occur in episodes.
PRP therapy for osteoarthritis
Osteoarthritis is a degenerative disease of the joints. There are various therapies that can alleviate the suffering of osteoarthritis. One of them is autohemotherapy, which we offer in our private practice.




